Scientific research highlights the significant influence of gut microbiota on the effectiveness of cancer immunotherapy, offering new strategies to overcome tumour resistance.
Cancer immunotherapy, particularly immune checkpoint inhibitors (ICIs), functions by blocking immune-suppressive molecules such as PD-1, PD-L1, and CTLA-4, allowing immune cells to target and destroy tumours. However, with a success rate of less than 50%, researchers are investigating factors that impact treatment outcomes. Since 2015, studies in mice have demonstrated that gut microbiota plays a crucial role in enhancing the response to ICI therapy, providing a potential avenue for therapeutic improvements.
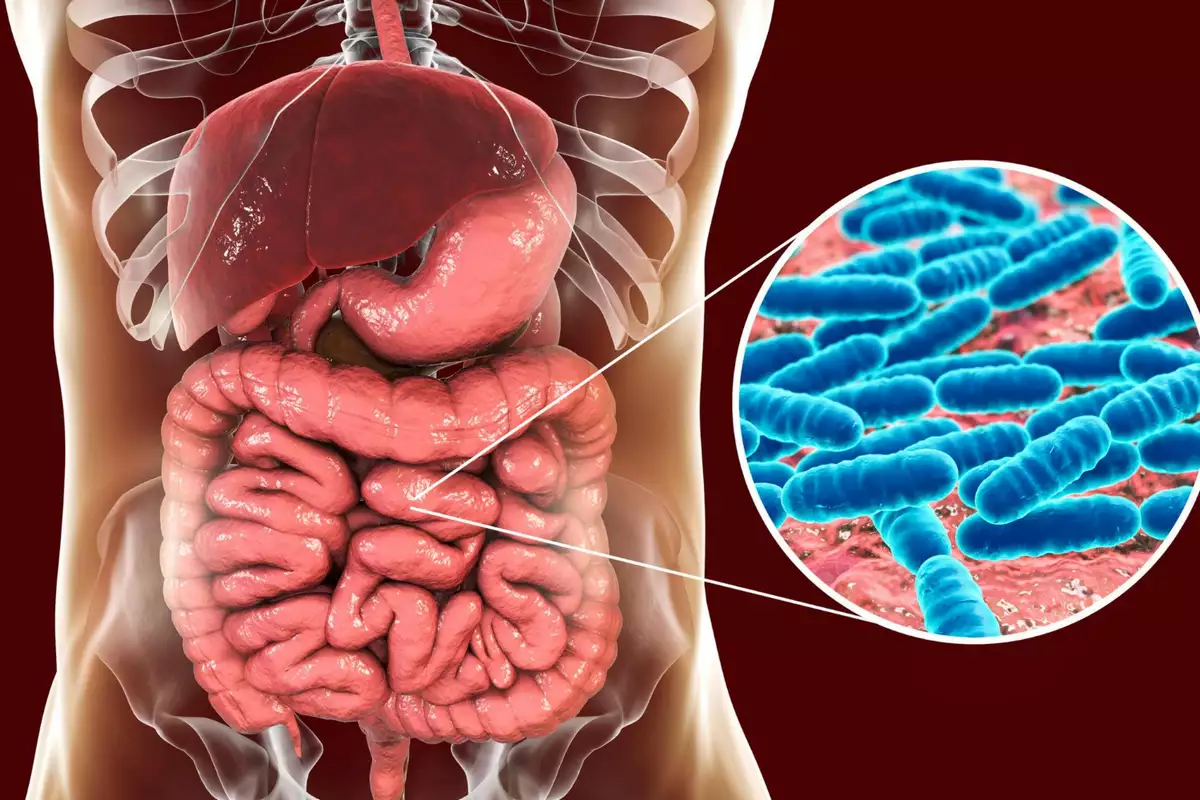
Specific bacterial consortia, including Bifidobacterium, Clostridiales, and individual strains such as Bifidobacterium longum, Akkermansia muciniphila, and Faecalibacterium prausnitzii, have been identified as positive modulators of immune response. These bacteria enhance CD8+ T cell activation and interferon-γ (IFN-γ) production, key mechanisms in anti-tumour immunity. Bacterial metabolites like inosine, indole-3-aldehyde, and butyrate also contribute to immunotherapy effectiveness by influencing tumour-immune interactions, making them promising targets for new treatment strategies.
Clinical studies in patients with non-small cell lung cancer, melanoma, and other malignancies further confirm the microbiota’s role in predicting immunotherapy outcomes. The presence of Akkermansia muciniphila, Faecalibacterium, and Enterococcus faecium correlates with improved treatment response. Additionally, faecal microbiota transplantation (FMT) from patients who respond well to ICIs into non-responders has shown potential in enhancing therapeutic efficacy.
However, antibiotics negatively impact immunotherapy by depleting beneficial bacteria and promoting immune-suppressive microbial populations. Research indicates that antibiotic use is linked to poorer outcomes in lung cancer, renal cell carcinoma, and triple-negative breast cancer. Probiotic interventions, such as Clostridium butyricum, show promise, though some Bifidobacterium-based probiotics may paradoxically promote tumour growth.
Investigations into bacterial metabolites as therapeutic agents offer another promising approach. For instance, Lactobacillus gallinarum produces indole-3-carboxylic acid, which suppresses regulatory T cells and enhances CD8+ T cell activation, while Coprobacillus cateniformis reduces PD-L2 levels, boosting PD-1/PD-L1 blockade effectiveness.
Understanding the intricate relationship between gut microbiota and immune function presents new opportunities for optimizing cancer immunotherapy. Ongoing research aims to identify key bacterial strains and metabolites that could serve as adjunct therapies, ultimately improving treatment outcomes and overcoming tumour resistance.






